In a landmark achievement for the fight against HIV, Sweden has attained the critical “95-95-95” target on the path to tackling the disease. Advanced bioinformatics modeling developed by a team from Los Alamos National Laboratory was deployed to track and verify the country’s progress toward the Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization target.
The 95-95-95 goal refers to 95% of all people with HIV in a population having received a diagnosis, 95% of diagnosed people having received treatment, and 95% of treated people having had their treatment been effective enough to result in unmeasurable virus levels. Sweden now reports 96% diagnosis, 99% of the diagnosed receiving treatment, and 98% of the treated seeing virus suppression to unmeasurable levels.
“This achievement is a monumental moment for public health,” said Thomas Leitner, Los Alamos researcher and leader of the Lab’s HIV modeling program. “Our team at Los Alamos is proud to contribute the advanced modeling that has helped further the efforts to reach these targets. Being able to track the incidence and prevalence of HIV is essential in combatting the disease with effective prevention and treatment.”
Sweden’s progress on the 95-95-95 target is the first such effort to be confirmed and described in peer-reviewed literature. A paper in which Los Alamos authors were joined by peers in the Swedish medical, public health and academic communities was recently published in the prestigious journal Eurosurveillance, the official journal of the European Center for Disease Prevention and Control.
A model for incidence and prevalence
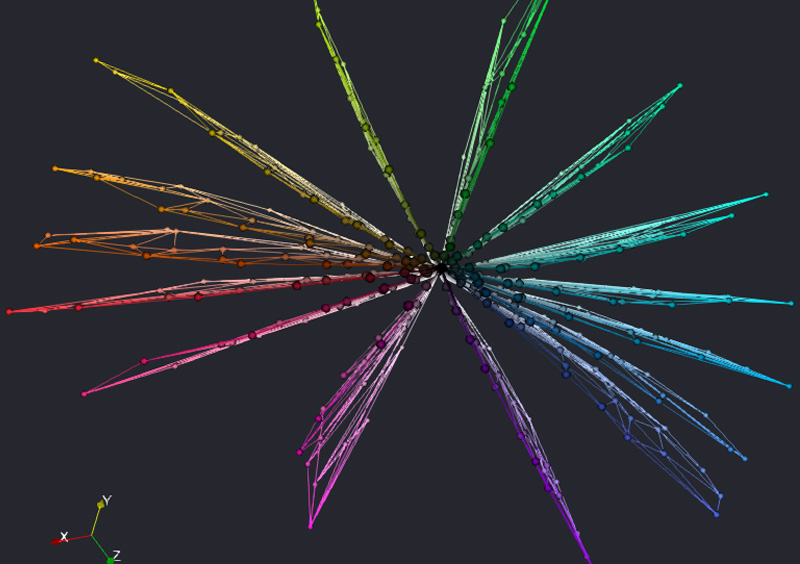
The modeling team took on the challenge of estimating how many people in Sweden live with HIV infection; many people may be unaware of their status for years before an official diagnosis. The team used a comprehensive clinical database — all identifying information such as names, birthdays and addresses being completely anonymized — to determine the number of people infected per year (incidence) as well as the number currently living with the disease in Sweden (prevalence), diagnosed or not.
To arrive at HIV incidence, the team used biomarkers including a cell count estimating a target cell population known to go down over the course of HIV infection, as well as an estimate of the number of mutations of the HIV virus in the body. The model combines those two biomarkers to estimate time since infection. From there, the model can determine incidence — the number of diagnosed persons of all that were infected in a year. A robust public health program will diagnose a high percentage of infected people, and that is exactly what Sweden achieved, with 96% in the key first 95 of the 95-95-95 target.
“For public health programs such as the attempted elimination of HIV in a country, it is very important to know how large the epidemic is in a given year,” Leitner said. “You need that fundamental measure to assess if prevention attempts such as isolation, vaccinations, behavioral interventions and so forth are working. If the prevention you’re doing is working, incidence and prevalence should go down.”
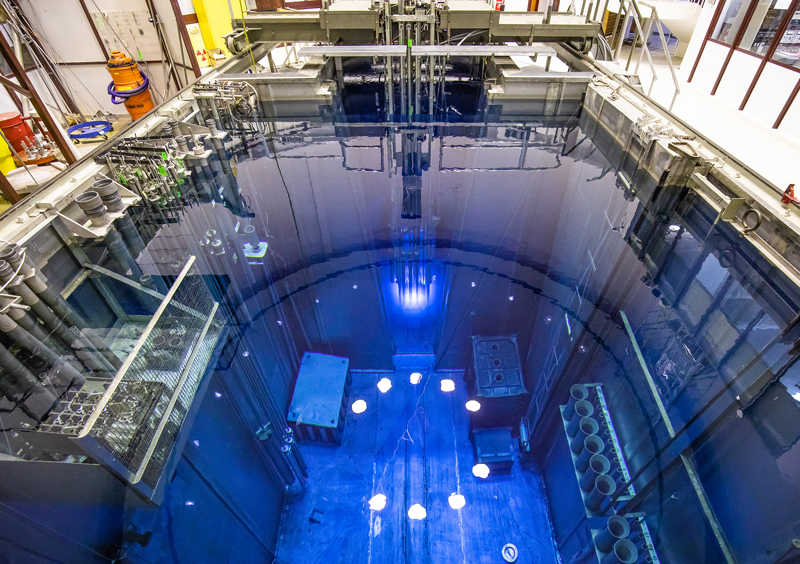
A publicly available model
The model created by Leitner and his team — the entire code — is publicly available on GitHub. Users with a comprehensive and high-quality data set can apply the methodology to their country, town or other population.
Leitner’s team will continue to work on the modeling in collaboration with Swedish public health efforts, for instance, in understanding the origin of virus cases among native and migratory populations. He also anticipates approaching American authorities on how modeling can contribute to combating HIV through programs such as the Centers for Disease Control and Prevention’s Ending the HIV Epidemic in the U.S. program.
Paper: “Sweden surpasses the UNAIDS 95-95-95 target: estimating HIV-1 incidence, 2003 to 2022.” Eurosurveillance. DOI: 10.2807/1560-7917.ES.2024.29.42.2400058
Funding: The research is supported in the U.S. by the National Institutes of Health.
LA-UR-24-31485
Contact
Brian Keenan | (505) 412-8561 | bkeenan@lanl.gov